A. B. Chagpar1, N. Horowitz1, B. Killelea1, T. Tsangaris2, M. Butler1, K. Stavris1, V. Bossuyt1, M. Harigopal1, F. Li1, X. Yao1, S. Evans1, E. Hofstatter1, T. Sanft1, D. Lannin1, M. Abu-Khalaf1, L. Wilson1, L. Pusztai1 2Thomas Jefferson University,Surgery,Philadelphia, PA, USA 1Yale University,New Haven, CT, USA
Introduction: Obtaining negative margins at partial mastectomy (PM) is often seen as being consistent with adequate resection; however, some women with negative margins have occult disease remaining in the breast. We sought to identify factors that are associated with such occult disease.
Methods: The SHAVE trial is a prospective randomized controlled trial in which 235 women with stage 0-3 disease undergoing PM were randomized intraoperatively to either have routine cavity shave margins (CSM) taken at the time of initial surgery (n=119), or not (n=116). The 76 women randomized to the ‘shave’ arm of the trial who had negative margins prior to randomization formed the cohort of interest for this analysis. Patients who were found to have occult cancers in the CSM were compared to those with no further disease. Non-parametric statistical analyses were performed using SPSS Version 21.
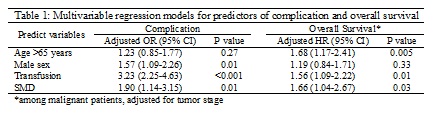
Results: Of 76 patients with negative margins prior to randomization to the ‘shave’ group, 9 (11.8%) had occult cancers found in the CSM. Six of these patients had occult DCIS, two had occult invasive disease, and one had both. The median extent of DCIS and invasive cancer found in the CSM was 0.25 cm (range; 0.05 – 0.80 cm) and 0.30 cm (range; 0.17-0.30 cm), respectively. Neither volume of tissue excised prior to CSM nor that of the CSMs was correlated with occult disease (p=0.52 and p=0.80, respectively). Patient age, race, tumor size, grade, hormone receptor status, LVI, lymph node status, and use of neoadjuvant chemotherapy similarly could not predict occult disease (all p>0.05; see table for selected parameters). However, the presence of invasive lobular cancer (ILC) trended towards association with the finding of occult disease in initially margin-negative patients (p=0.06).
Conclusion: Nearly 12% of patients with negative margins at PM will have occult disease; patients with ILC are more likely to have such occult disease. The impact of such disease on locoregional recurrence, however, remains to be elucidated.