C. M. Papageorge1, G. D. Kennedy1 1University Of Wisconsin,Department Of Surgery,Madison, WI, USA
Introduction: Anemia is an independent predictor of worse postoperative outcomes, however blood transfusion also has known associated risks such as worse cancer outcomes and immune suppression. In this study, we tested the hypothesis that perioperative blood transfusion is an independent risk factor for postoperative complications following colectomy.
Methods: Patients undergoing colectomy from 2012-2013 were selected from the National Surgical Quality Improvement Program (NSQIP) targeted colectomy participant use file. Exclusion criteria included unavailability of preoperative hematocrit value, emergent operations, and ASA Class 5. Patients were divided into four groups based on receipt of perioperative blood transfusion: no transfusion, preoperative transfusion only, intra/postoperative transfusion only, or both. Univariate analysis using Chi-squared tests was performed to compare rates of postoperative complications between the four groups. Propensity scores were calculated separately for receipt of preoperative transfusion and intra/postoperative transfusion. Multivariate analysis was then performed utilizing a propensity score-adjusted multiple logistic regression model to predict 30-day postoperative complications.
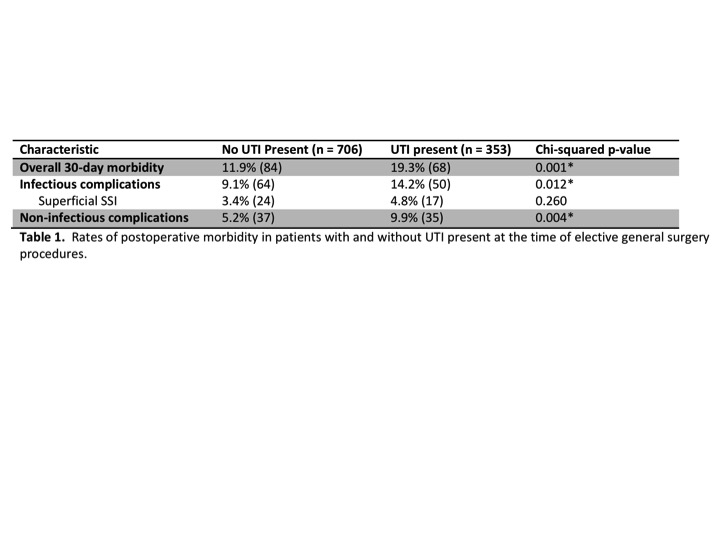
Results: A total of 30,680 patients were included in the study, with an overall transfusion rate of 11.6% (n = 3572). On univariate analysis, transfusion was associated with significantly higher rates of postoperative morbidity (Table 1). The risk-adjusted multivariate model confirmed an increased risk of postoperative morbidity associated with preoperative transfusion alone (OR 1.36, 95% CI 1.09-1.71), with intra/postoperative transfusion alone (OR 2.11, 95% CI 1.92-2.31), and with both (OR 2.40, 95% CI 1.82-3.16). When examining the impact of timing of transfusion, intra/postoperative transfusion was independently associated with a higher risk of postoperative morbidity compared to preoperative transfusion (OR 1.55, 95% CI 1.23-1.95). Finally, preoperative transfusion is not associated with a significant change in 30-day postoperative complications in the setting of either mild/moderate anemia (OR 1.17, 95% CI 0.91-1.50) or severe anemia (OR 1.47, 95% CI 0.84-2.59).
Conclusion: In this study, we found that transfusion is an independent predictor of postoperative complications. While it is clear that sicker patients tend to receive transfusions, these findings suggest that at a minimum, transfusion is a marker of worse surgical outcomes, and possibly even contributes to postoperative morbidity. Furthermore, based on this retrospective data, anemic patients do not appear to benefit from preoperative transfusion, and therefore empiric preoperative transfusion may be exposing the patient to unnecessary risks.