O. Al-Kathiri1, S. Y. Salim1, L. M. Warkentin1, A. Gallivan3, P. Tandon4, T. A. Churchill1, V. E. Baracos3, R. G. Khadaroo1,2 1University Of Alberta,Div. General Surgery/ Dept. Surgery,Edmonton, ALBERTA, Canada 2University Of Alberta,Div. Critical Care Medicine/ Dept. Surgery,Edmonton, ALBERTA, Canada 3University Of Alberta,Department Of Oncology,Edmonton, ALBERTA, Canada 4University Of Alberta,Div. Gastroenterolgy/ Dept. Medicine,Edmonton, ALBERTA, Canada
Introduction: Sarcopenia was identified as the loss of muscle mass and function that occurs with aging. It has been associated with high morbidity and mortality in patients over 65 years. Yet it is not part of the routine screening process in geriatric care. Computed tomography (CT) scan at the lumbar site L3 has been used as the gold standard tool to identify sarcopenia. Unfortunately high cost, limited availability, and radiation exposure limits the use of CT. We propose ultrasonography (US) of the thigh muscle as a possible objective, feasible, reproducible, portable, and risk free tool that can evaluate sarcopenia. The aim of this study was to evaluate US as a tool for the assessing sarcopenia in elderly patients.
Methods: We recruited 38 patients over 65 years old, referred to the Acute Care Surgery service. Using Sonosite US, thigh muscle thickness (measured at the midpoint between the greater trochanter, 10cm below and lateral to ASIS) was standardized to patient height. CT scan images at L3 were analyzed through SliceOmatic. Skeletal muscle index was calculated using skeletal muscle surface area. Sarcopenia was defined as skeletal muscle index < 41cm2/m2 for females and <43cm2/m2 or < 53cm2/m2 for males (with BMI <25kg/m2 or >25kg/m2, respectively). Rockwood Clinical Frailty score (1-3 non frail, >4 frail) was used to assess patient condition.
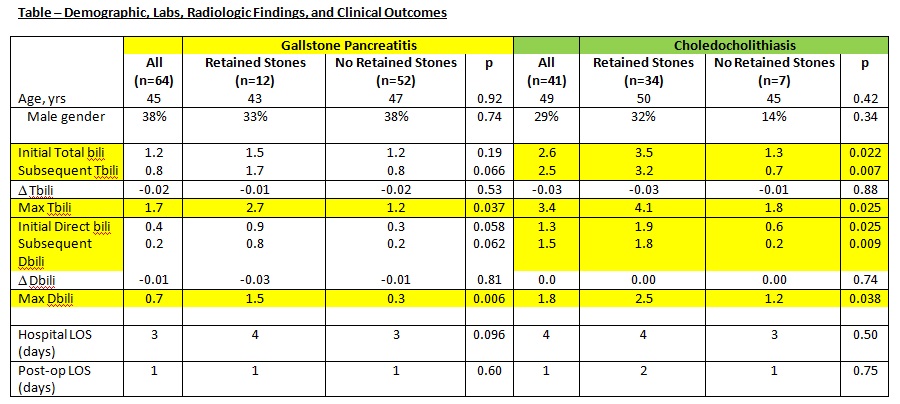
Results: The mean age of our preliminary study group was 78 ± 8 years and 68% (n=26) were females. Demographic, body composition, US and CT data of patients are described in Table 1. Sarcopenia was identified through CT in 69% of the patients. Sarcopenic patients had a greater number of in-hospital complications (48% vs 16.6% in non-sarcopenic, p =0.0001). There was no difference in duration of stay between sarcopenic and non-sarcopenic patients (14 vs 11 days, p=0.06). There were significant differences between sarcopenic and non-sarcopenic females in skeletal muscle surface area (113 ± 9 versus 91 ± 10 cm2, p < 0.001), and skeletal muscle index (35.2 versus 46.3 cm2/m2, p< 0.001). CT scan skeletal muscle index of sarcopenic patients showed significant correlation with frailty score (r2=0.21, p<0.05). US of rectus femoris in females was significantly associated with frailty score (r2=0.19, p=0.008). The receiver-operating characteristic (ROC) for thigh ultrasound was not able to distinguish sarcopenic patients (area ROC curve=0.6, p=0.8).
Conclusion: CT identified sarcopenia was associated with high-risk frail patients. US measured muscle thickness was predictive of frailty but not of CT identified sarcopenia. Further patient recruitment with thigh US is needed to determine the sensitivity of the use of US in screening for sarcopenia.