B. F. Gilmore1, A. K. Brys2, N. S. Nath2, K. L. Rialon1, M. E. Barfield1, G. Pomann3, L. Ding3, J. Migaly1, P. J. Mosca1 1Duke University Medical Center,Department Of Surgery,Durham, NC, USA 2Duke University School Of Medicine,Durham, NC, USA 3Duke University,Department Of Bioinformatics And Biostatistics,Durham, NC, USA
Introduction:
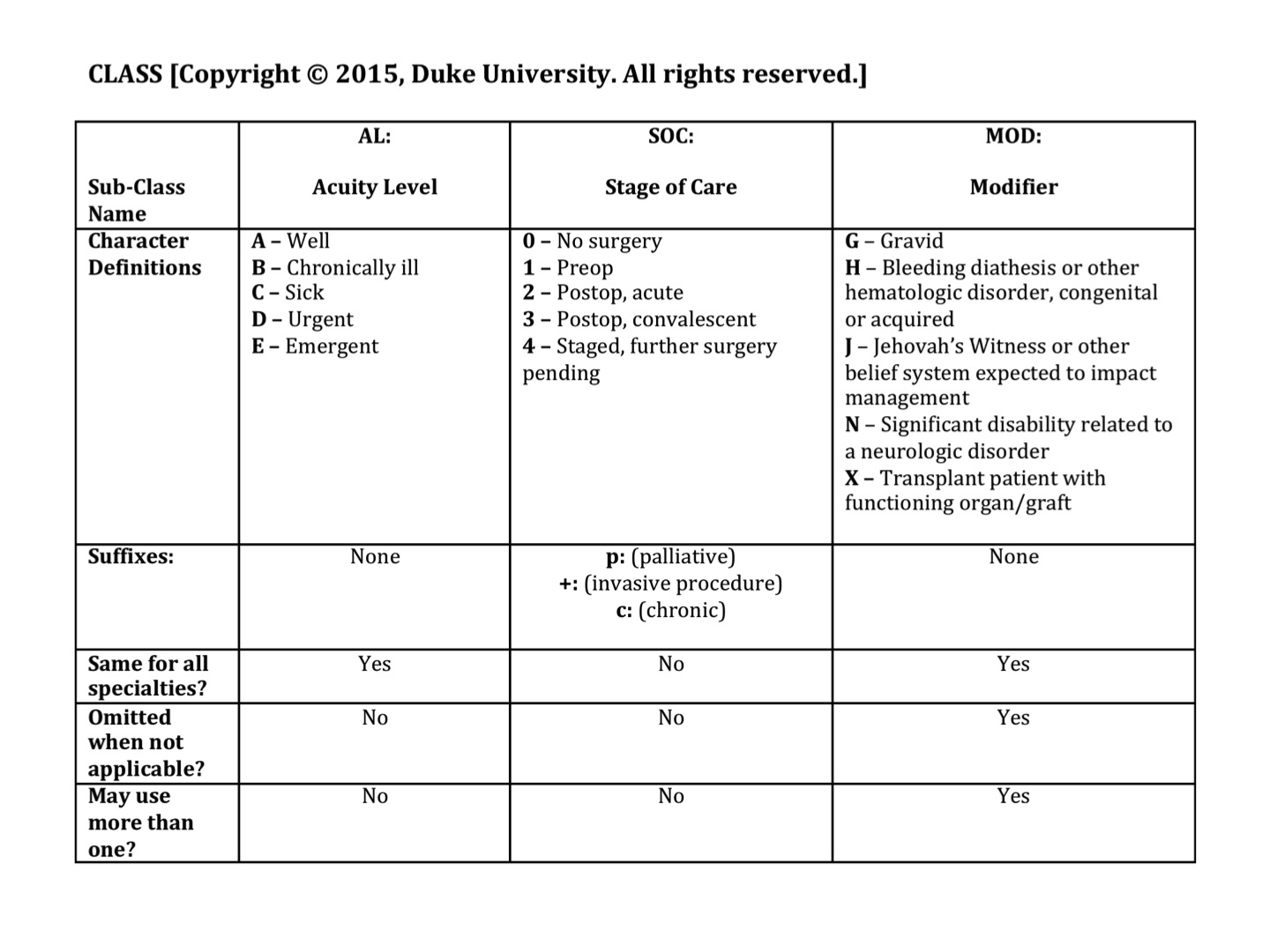
The handoff of medical information from one provider to another can be inefficient and error-prone, potentially undermining patient safety. Though several tools for structuring handoffs exist, none provide a concise, standardized framework for ensuring that patient acuity is efficiently and reliably communicated. This prompted the development of a novel tool, the Clinical Acuity Shorthand System (CLASS) for Surgery. This is a patient classification system that incorporates the acuity and severity of illness, phase of care, and key comorbidities into a score that can be used during transitions of care to summarize the overall wellness of the patient and convey the need for additional interventions.
Methods:
Surgical trainees at a single center were asked to complete a voluntary, anonymous exam in which a novel patient classification system would be applied to 10 theoretical patient scenarios. Responses were scored on the accuracy of classification compared to target answers. Performance was evaluated overall and between groups of trainees; time required to complete the examination was also measured. Following completion of this exercise, respondents were surveyed regarding perceived utility of the system with regard to preventing medical errors and improving efficiency.
Results:
The study task was completed by 17 participants. Mean time from first exposure to the system to completion of the application task was 10.3 ± 8.4 minutes. Interns and junior residents were able to apply the system with comparable accuracy, and in fact exceeded the accuracy of senior residents. Most respondents indicated that such a system would be feasible to institute and could prevent medical errors arising from communication breakdowns.
Conclusion:
CLASS is a novel classification system that can be learned quickly and implemented readily by trainees, and can be used to convey key patient information concisely and with acceptable fidelity regardless of level of training. Further studies are necessary to determine whether CLASS has the potential to decrease the rate of communication-related medical errors during handoff.