N. Amini1, G. A. Margonis1, S. Buttner1, S. Besharati2, Y. Kim1, F. Gani1, F. Sobhani2, I. R. Kamel2, T. M. Pawlik1 1Johns Hopkins University School Of Medicine,Surgery,Baltimore, MD, USA 2Johns Hopkins University School Of Medicine,Radiology,Baltimore, MD, USA
Introduction: Obese patients may present with several metabolic abnormalities including hyperglycemia, hyper-insulinemia, and hyperlipidemia. These metabolic perturbations, as well as increased production of cytokines from visceral adipose tissue, negatively affect hepatocyte proliferation. Data on the impact of obesity on liver regeneration after major liver hepatectomy are lacking. As such, we sought to compare the liver volume regeneration index (RI) among patients by body mass indexes (BMI).
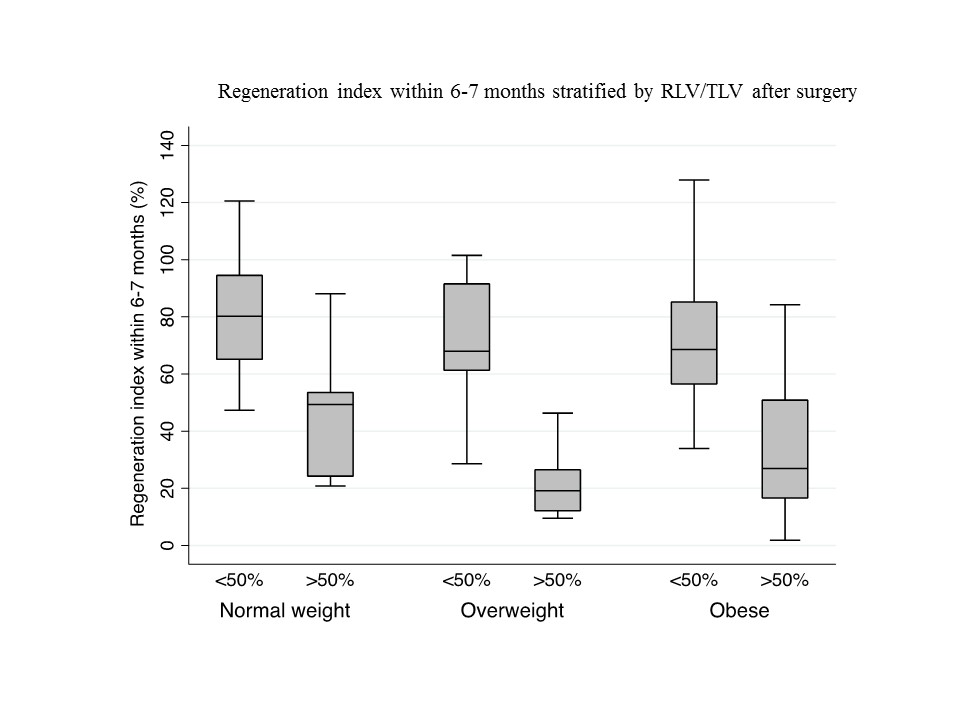
Methods: : Patients undergoing a major hepatectomy (≥3 segments) between July 2004 and April 2015 with available pre- and postoperative computed tomographic (CT) scans were identified. Patients were stratified by preoperative BMI; normal BMI (<25), overweight (25-29), and obese (≥30). Patients were matched on the number of segments resected, as well as the remnant liver volume (RLV) to total liver volume (TLV) ratio. TLV was assessed preoperatively, while RLV was measured at 2-3 and 6-7 months after surgery. The resected volume at surgery was subtracted from TLV to define postoperative RLV (RLVp). The liver volume RI was defined as the relative increase within 2-3 months [(RLV2-3m-RLVp)/RLVp] and 6-7 months [(RLV6-7m-RLVp)/RLVp] after surgery.
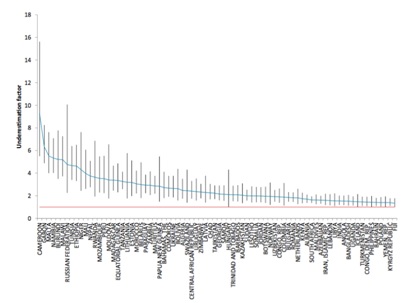
Results:Among a matched cohort of 80 patients, median age was 58 years (IQR, 49.7-68.6) and most were male (53.8%). Of note, while clinicopathological characteristics were similar across the three groups, obese patients presented with a higher incidence of diabetes (normal, 10% vs. overweight, 33.3% vs. obese, 46.2%; P=0.01). 48.7% of patients underwent a right hepatectomy while 25.0% and 26.3% underwent a left or extended hepatectomy, respectively. Obese patients had a higher median blood loss (normal, 300cc vs. overweight, 500cc vs. obese, 800 cc; P<0.001) and were more likely to be transfused (normal; 3.9% vs. overweight; 13.6% vs. obese; 30.4%, P=0.04). Initial postoperative RLVp/TLV was comparable across BMI categories (normal, 55.3% vs. overweight, 69.4% vs. obese, 67.8%, P=0.43). While BMI did not impact the RI within the first 2-3 months (normal weight, 32.5% vs. overweight, 24.7% vs. obese, 31.9% cc; P=0.60), the RI at 6-7 months was lower among overweight and obese patients (normal weight, 66.0% vs. overweight, 25.2% vs. obese, 47.9%, P=0.04, Figure).
Conclusion:Following major hepatic resection, BMI did not impact short-term liver regeneration over the initial 2-3 months. In contrast, liver regeneration assessed at 6-7 months was lower among overweight and obese patients compared with normal weight patients. Further research is necessary to investigate the metabolic factors and cytokine pathways that may influence long-term liver regeneration.