D. C. Cron1, M. J. Englesbe1, K. L. Carrier3, C. Bolton2, M. Joseph2, S. Moser2, J. F. Waljee1, P. E. Hilliard2, S. Kheterpal2, C. M. Brummett2 1University Of Michigan,Surgery,Ann Arbor, MI, USA 2University Of Michigan,Anesthesiology,Ann Arbor, MI, USA 3University Of Michigan,College Of Pharmacy,Ann Arbor, MI, USA
Introduction:
Opioids are increasingly used to manage chronic pain, and chronic opioid users are among the most challenging patients to care for perioperatively. Given the epidemic of opioid-related morbidity and mortality, it is critical to understand how opioid use impacts surgical outcomes. In this context, we examined the effect of preoperative opioid use on clinical and financial outcomes in adults undergoing major elective abdominal surgery.
Methods:
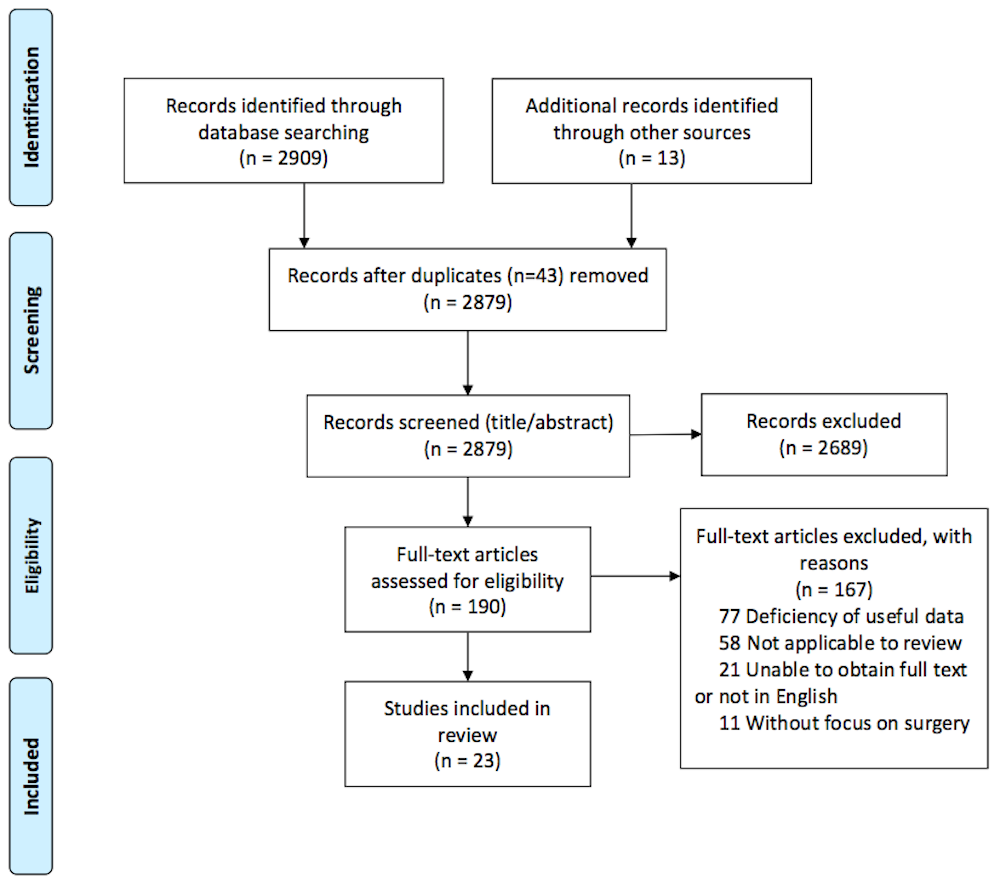
We retrospectively reviewed 2460 patients drawn from a statewide surgical quality collaborative database who underwent elective abdominopelvic surgery at a single center between 2008-2014. We identified preoperative opioid use from the medical record at the anesthesia preoperative evaluation (day of operation). Opioid use was categorized first as any opioid use (binary) and then as none vs. short-acting only vs. long-acting +/- short-acting. Outcomes included 90 day total hospital costs, hospital length of stay (LOS), discharge destination, 30 day hospital readmissions, and 30 day major complication rates. Standard multivariate regression techniques were used to adjust for case complexity and patient-specific risk factors (age, ASA class, functional status, smoking, medical comorbidities).
Results:
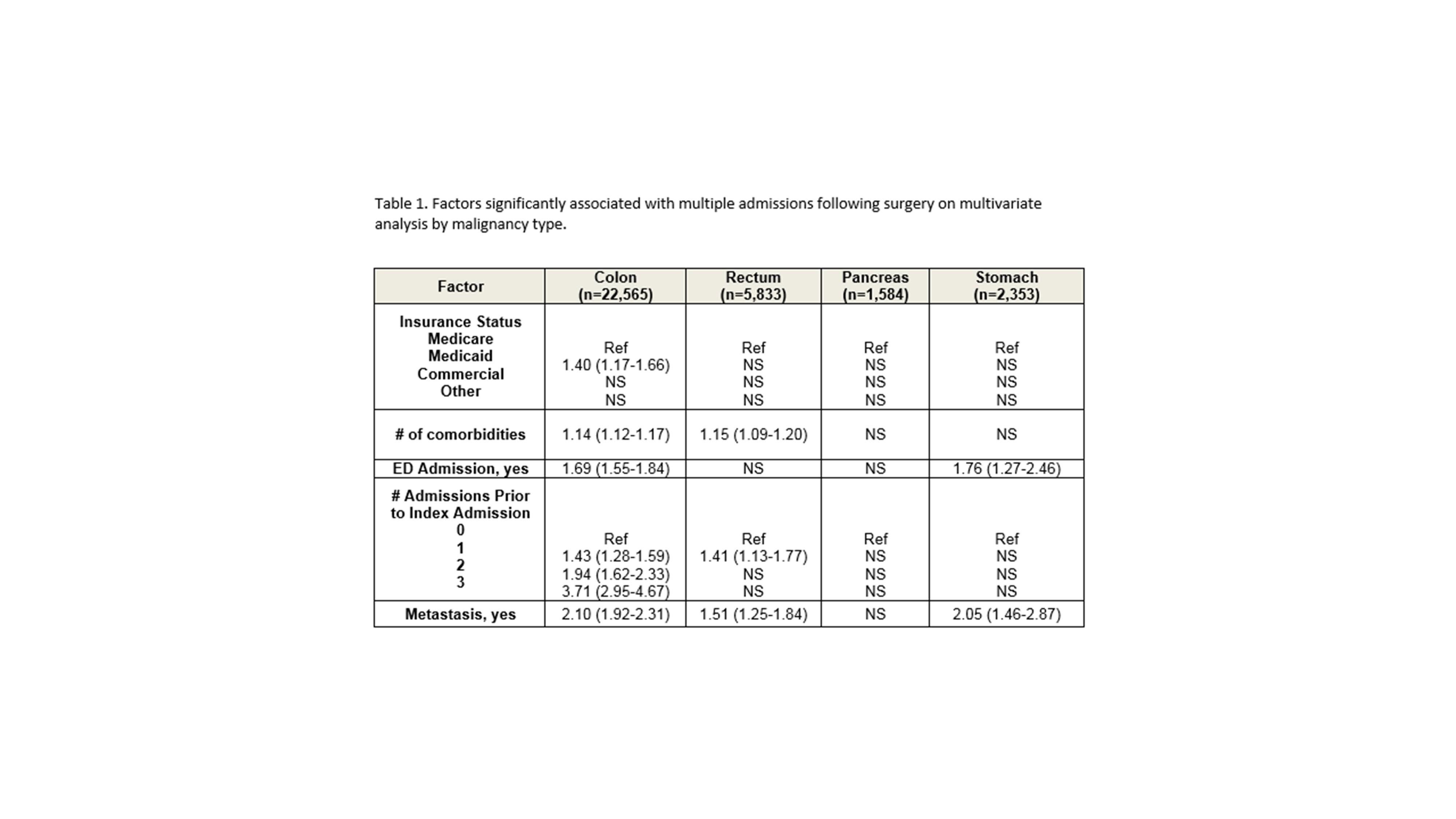
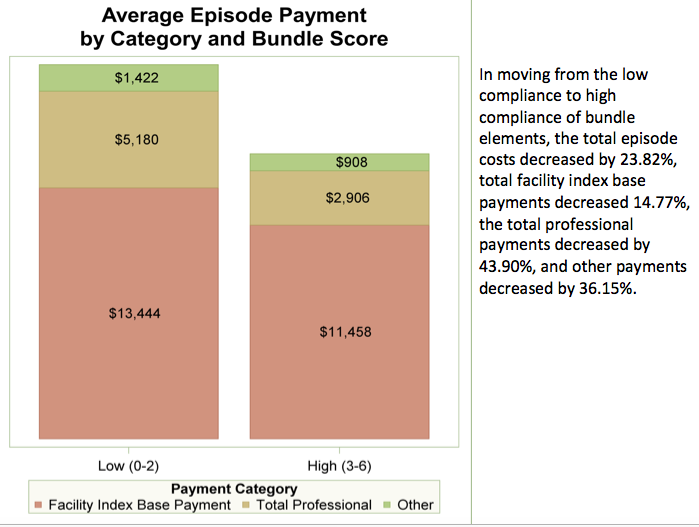
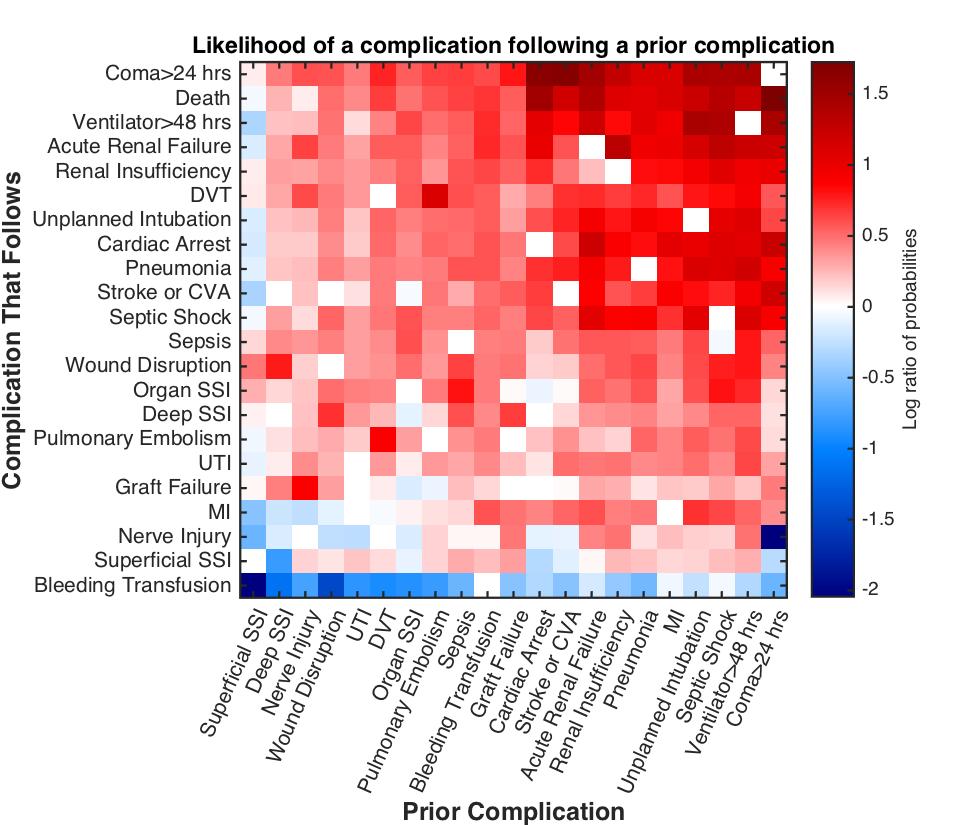
497 patients (20%) used opioids preoperatively. After covariate adjustment, opioid users (compared to opioid-naïve) had higher mean costs ($27091 vs. $24307, P<0.01), longer mean LOS (6.0 vs 5.2 days, P<0.01), increased readmissions (10% vs 6%, P<0.01), higher complication rates (20% vs. 16%, P=0.04), but there was no significant difference in non-home discharge rates (14% vs. 11%, P=0.11). Surgical site infection, sepsis, and postop transfusion were significantly more common in opioid users. When categorized by short vs. long-acting opioids, both levels of opioid use were significantly associated with costs, LOS, and readmissions in multivariate analyses. The effect of long-acting opioids was stronger than that of short-acting opioids across all outcomes (except discharge destination). The figure shows a stepwise increase in adjusted mean costs and LOS across categories of opioid use, with long-acting opioid users having the highest costs and LOS.
Conclusion:
Opioid use is common prior to abdominal surgery and is associated with increased healthcare utilization and morbidity, even after risk-adjustment. Preoperative opioids represent a potentially modifiable risk factor and a novel target for surgical quality improvement. Going forward, strategies to reduce opioid use and implement alternative pain management options may improve the quality and value of surgical care in this vulnerable patient population.