C. Lee1,4, A. Deal4, P. A. Ubel2, R. Hugh1, L. Blizard3, K. R. Sepucha3, Y. Liu1, D. Ollila1,4, M. P. Pignone1,4 1University Of North Carolina At Chapel Hill,Chapel Hill, NC, USA 2Duke University,Fuqua School Of Business,Durham, NC, USA 3Harvard School Of Medicine,Brookline, MA, USA 4Lineberger Comprehensive Cancer Center,Chapel Hill, NC, USA
Introduction: Breast reconstruction after mastectomy has the potential to improve patient reported outcomes. Prior studies have been limited by retrospective, cross-sectional designs and lack of controls, and most have not assessed patient decision making. We evaluated outcomes of reconstruction in a prospective, longitudinal, controlled study and examined whether informed choice was associated with outcomes.
Methods: Adult women undergoing mastectomy for stage 0-III breast cancer or prophylaxis were enrolled at a single site and surveyed before surgery and at 12 months. Decision making was assessed with the Decision Quality Instrument, rating and ranking scales, and conjoint analysis. Making an ‘informed choice’ was defined as having at least 50% knowledge and treatment concordant with preferences. Satisfaction w/ breasts, psychosocial well-being (WB), sexual WB, and physical WB of the chest were measured with the BreastQ (range 0-100). Decisional outcomes were measured with the Satisfaction with Decisions and Decision Regret scales. Baseline scores were compared using t-tests. Preference concordance was assessed with a kappa score. Multivariable linear regression was used to examine differences (by treatment and by informed choice) in patient-reported outcomes at 12 months, adjusting for baseline values, demographics, and clinical characteristics.
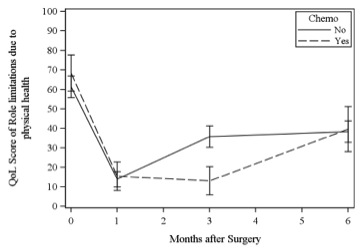
Results: 126 patients enrolled (83% participation); 111 completed baseline and 12 mo surveys. The immediate reconstruction rate was 44% (15 delayed reconstruction cases were excluded to simplify analysis). Patients having reconstruction were more likely to be white (88 vs. 69%, p=0.05), partnered (81 vs. 49%, p=0.002), or college educated (95 vs. 76%, p=0.01), and less likely to have adjuvant therapy (17 vs. 65%, p<0.01). Mean age was 54 and did not differ by treatment. Mean knowledge was 57%. 63% of patients had treatment that was concordant with preferences. 43% of patients made an informed choice. Satisfaction with breasts, sexual WB, psychosocial WB, and physical WB-chest declined from baseline to 12 mos, regardless of reconstruction. On multivariable analysis and adjusting for baseline values, reconstruction was associated with higher satisfaction w/ breasts (beta 13.1, p=0.008) at 12 mos; it was not associated with change in sexual WB (p=0.07), psychosocial WB (p=0.16) or physical WB (p=0.61). Informed choice was not associated with higher psychosocial WB (p=0.20), decision satisfaction (p=0.57), or decision regret (p=0.77).
Conclusion: Patients having mastectomy-only are different at baseline from patients having reconstruction. Both groups experienced decline in all well-being scores after surgery. Reconstruction was associated with higher satisfaction with breasts at 12-mos, but not with higher sexual, psychosocial, or physical WB. Informed choice was not associated with better outcomes, and most patients did not make an informed choice.