M. C. Zuniga1,2, G. Raghuraman1,2, E. Hitchner1,2, W. Zhou1,2 1VA Palo Alto Healthcare Systems,Vascular Surgery,Palo Alto, CA, USA 2Stanford University,Vascular Surgery,Palo Alto, CA, USA
Introduction: Monocytes and macrophages (MΦ) are key players in atherosclerotic plaque inflammation. Resistin has been associated with increased risk for cardiovascular complications but its mechanisms of action remain to be elucidated. We have previously observed higher levels of inflammatory cytokines in patients with ‘high’ resistin levels (4.97 – 13.3 ng/mL, AVE = 7.29), implicating that resistin may act through inflammatory pathways. In this study, we evaluated the direct effects of high levels of resistin on the monocyte/macrophage inflammatory state.
Methods: Monocytes were isolated from buffy coats of healthy controls, and some monocytes were differentiated into MΦ. Monocytes and MΦ were treated with resistin at a ‘high’ physiological level (10 ng/mL) with or without a selective PKC-ε inhibitor (1 µM). Monocytes/MΦ profiles were evaluated using immunocytochemistry (ICC) and verified with Western blot. CD80 and CD40 were used as markers for the M1 (pro-inflammatory) phenotype, and CD206 (mannose receptor) and CD163 were used for the M2 (anti-inflammatory) macrophage phenotype; CD14 and CD16 were used to assess monocyte states. Levels of resistin post-treatment were measured with ELISA. Data was analyzed with ANOVA, and a p-value of <0.05 was considered significant.
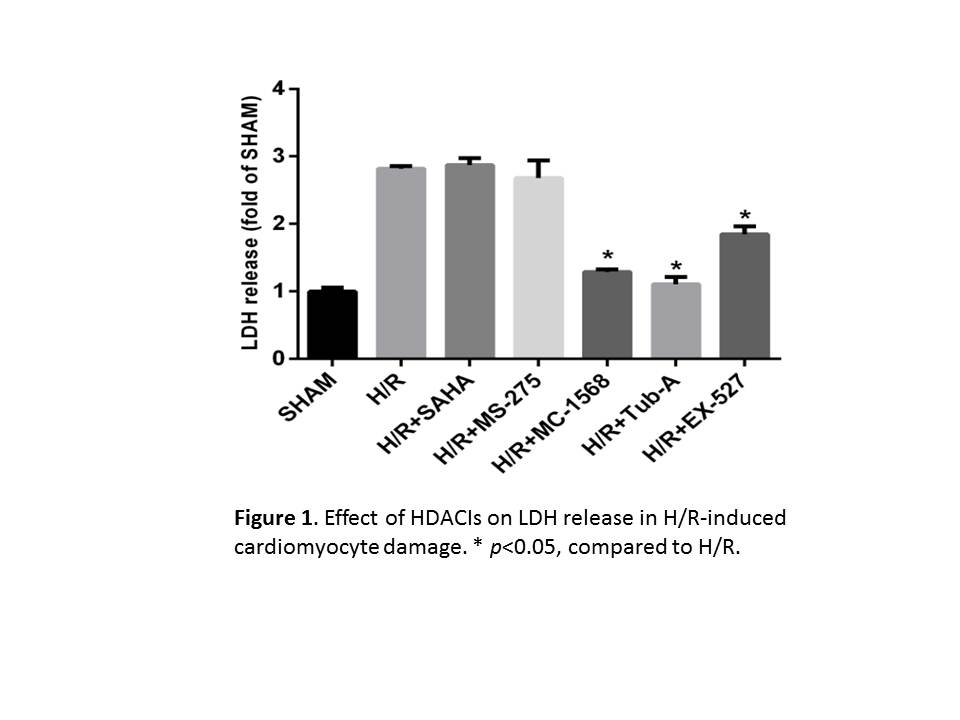
Results: Despite a very low basal expression of resistin (0.15 ng/mL), MΦ treated with resistin (10 ng/mL) showed significantly higher than expected production of resistin up to 18.2 ng/mL ± 1.17 (AVE ± SEM), suggesting a potential positive feedback mechanism in MΦ. This phenomenon was not observed in monocytes. ICC revealed that monocytes treated with resistin did not exhibit a change in CD14 or CD16 expression compared to the controls. Similarly, resistin-treated MΦ did not show significant changes in CD80 or CD163 expression. However, decreased CD206 and a markedly increased CD40 expression were observed (p<0.01). Western blot results confirmed these observations. Moreover, inhibition of PKC-ε mitigated resistin-induced CD40 upregulation (Figure 1 a, b, c).
Conclusion: Our study suggests that resistin stimulates MΦ toward a pro-inflammatory subtype through a positive feedback mechanism. PKCε-specific inhibition decreased CD40 up-regulation, highlighting a possible approach to prevent resistin-mediated M1 polarization and associated cardiovascular complications.