J. Kim1, Z. Sun1, B. C. Gulack1, E. Benrashid1, M. J. Miller2, A. C. Allori1, H. E. Rice1, C. K. Shortell1,2, E. T. Tracy1 1Duke University Medical Center,Surgery,Durham, NC, USA 2Duke University Medical Center,Radiology,Durham, NC, USA
Introduction:
With novel medical therapies, interventional procedures, and surgical techniques increasingly used to manage vascular anomalies, the quality of life for children with vascular anomalies has improved. This study aimed to define morbidities and costs related to modern-day care for children with vascular anomalies.
Methods:
We reviewed the 2003-2009 Kids’ Inpatient Database (KID) for pediatric patients (age < 21 years) hospitalized with hemangiomas, arteriovenous malformations (AVM), or lymphatic malformations (LM) as a primary diagnosis. Patients were grouped by type of vascular anomaly. Patient characteristics, comorbidities, complications, and hospital charges were compared.
Results:
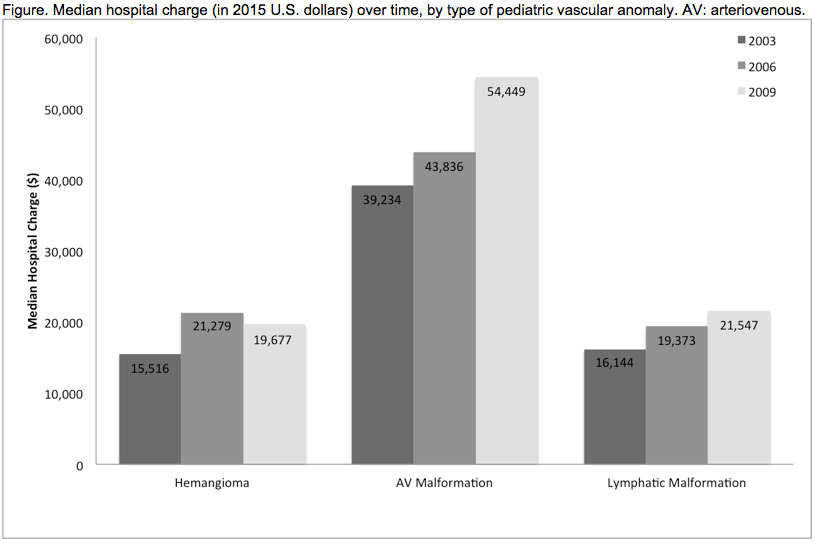
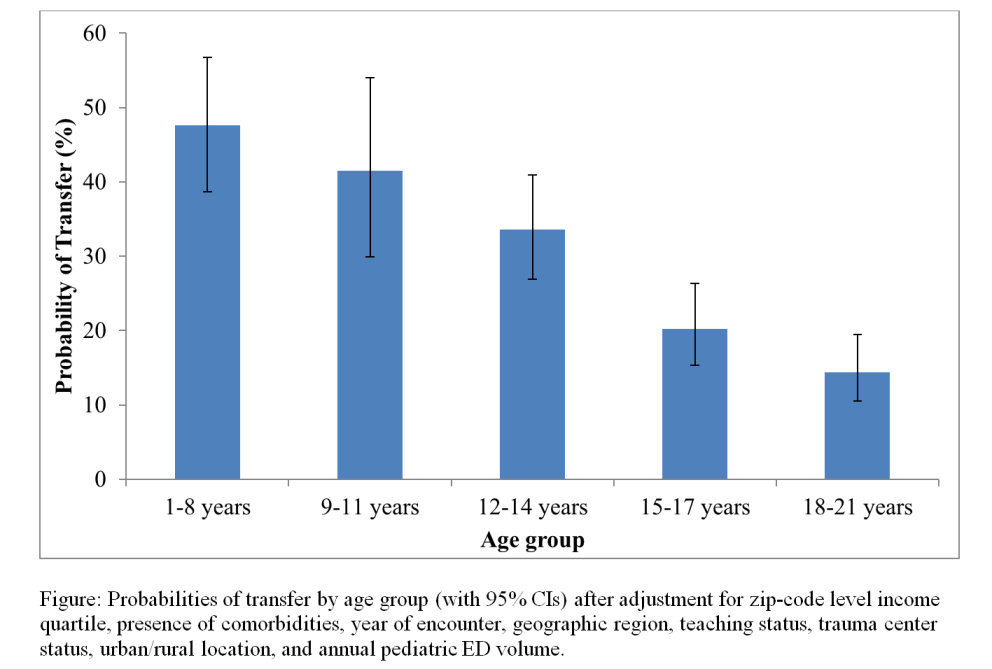
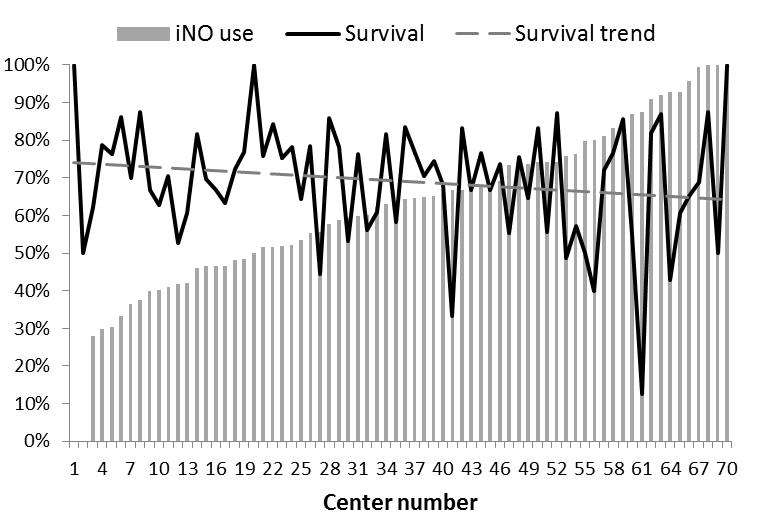
In total, 7,485 pediatric patients with vascular anomalies were identified. Within this cohort, frequently associated comorbidities included chronic anemia (4.0%), hypertension (2.4%), and coagulopathy (1.8%). They also had nontrivial rates of sepsis (4.6%) and cellulitis (1.4%) associated with hospital care. Notably, children with AVM had the highest rate of in-hospital mortality (1.0%, p < 0.001). AVM also were associated with the highest median hospital charge ($38,574, p < 0.001), more than twice the cost for hemangiomas or LM. AVM care also had the greatest increase in median hospital charge (38.8%) from 2003 to 2009 (Figure).
Conclusion:
We found a significant rate of morbidity in children with vascular anomalies, most often from blood loss and infection. The greater cost of AVM care may be related to the higher mortality rate as well as the complexity of procedures required to treat them. Cost-effective management of vascular anomalies should target prevention and early recognition of both chronic comorbidities and acute complications.