S. B. Bateni1, E. A. David2, R. J. Bold3, D. T. Cooke2, F. J. Meyers4, R. J. Canter3 1University Of California – Davis,General Surgery,Sacramento, CA, USA 2University Of California – Davis,Cardiothoracic Surgery,Sacramento, CA, USA 3University Of California – Davis,Surgical Oncology,Sacramento, CA, USA 4University Of California – Davis,Hematology/Oncology,Sacramento, CA, USA
Introduction: Although surgical intervention among patients with disseminated malignancy (DMa) carries high morbidity and mortality, recent single institution retrospective studies have demonstrated improvements in survival among advanced lung cancer patients and patients with lung metastases undergoing lung resection. We sought to evaluate the rates of acute morbidity and mortality following lung resection in stage IV cancer patients to further describe risks associated with such intervention.
Methods: For the years 2011-2012, we identified 6,360 patients from the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) undergoing lung segmentectomy, wedge resection, lobectomy, or pneumonectomy, including 603 patients (9.5%) with a diagnosis of DMa. Standard parametric and nonparametric statistical analyses were used to evaluate the 30-day morbidity and mortality associated with lung resection and compare outcomes among patients with and without DMa.
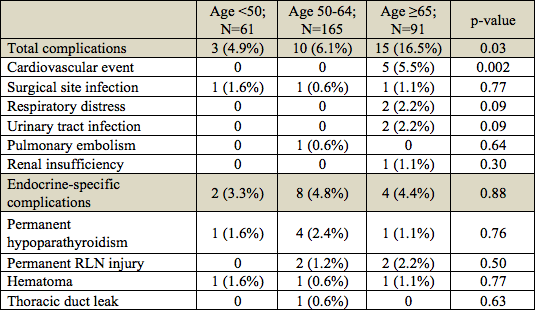
Results: Among DMa patients, 200 (33.2%) were diagnosed with primary lung cancer, 357 (59.2%) had metastases to the lung, and 46 (7.6%) were unspecified. Most DMa patients had independent functional status (99.2%) and were without any dyspnea symptoms (84.4%). Overall 30-day morbidity, serious morbidity and mortality for DMa patients were 12.1%, 7.6% and 1.8%, respectively, and 95.9% of patients were discharged home. DMa patients with a primary diagnosis of lung cancer had a significantly greater mortality compared to patients with lung metastases (3.5% vs. 0.6%, p < 0.01). Pneumonectomy among DMa patients had far worse overall morbidity, serious morbidity and mortality compared to other types of lung resections (28.6% vs 12.1%, 28.6% vs 7.6%, and 7.1% vs 1.8%, respectively, p < 0.05). Of most clinical significance, when comparing outcomes for DMa versus non-DMa, overall morbidity was lower among DMa patients (12.1% vs. 15.4%, p < 0.05) and there were no significant differences in serious morbidity (8.3% vs. 9.8%, p > 0.05) or mortality (1.8% vs. 1.8%, p > 0.05) for all lung resections. Subgroup analysis by segmentectomy, wedge resection, lobectomy and pneumonectomy also demonstrated no significant differences in rates of overall morbidity, serious morbidity and mortality for DMa versus non-DMa patients (p > 0.05 for all).
Conclusion: With the exception of pneumonectomy, DMa patients undergoing pulmonary resections experienced low rates of overall morbidity, serious morbidity, and mortality. Moreover, surgical outcomes for pulmonary resections were comparable among DMa and non-DMA patients. Taken together, these data suggest that lung resections may be performed safely on select patients with DMa with both primary lung cancer and pulmonary metastatic disease, with important implications for both symptom palliation and multimodality care.