V. X. Zhou1, M. Lolas1, T. T. Chang1 1University Of California – San Francisco,Surgery,San Francisco, CA, USA
Introduction: Liver transplantation is currently the only treatment for end-stage liver disease (ESLD) and is limited by the critical shortage of donor organs. Implantation of liver organoids generated ex vivo by three-dimensional (3D) culture techniques may serve as an adjunct or alternative to liver transplantation. Efficient high-engraftment methods of introducing organoids into the liver parenchyma have not been established. In this study, we aim to develop a reliable surgical technique to implant liver organoids into the liver and assess their ability to engraft and function.
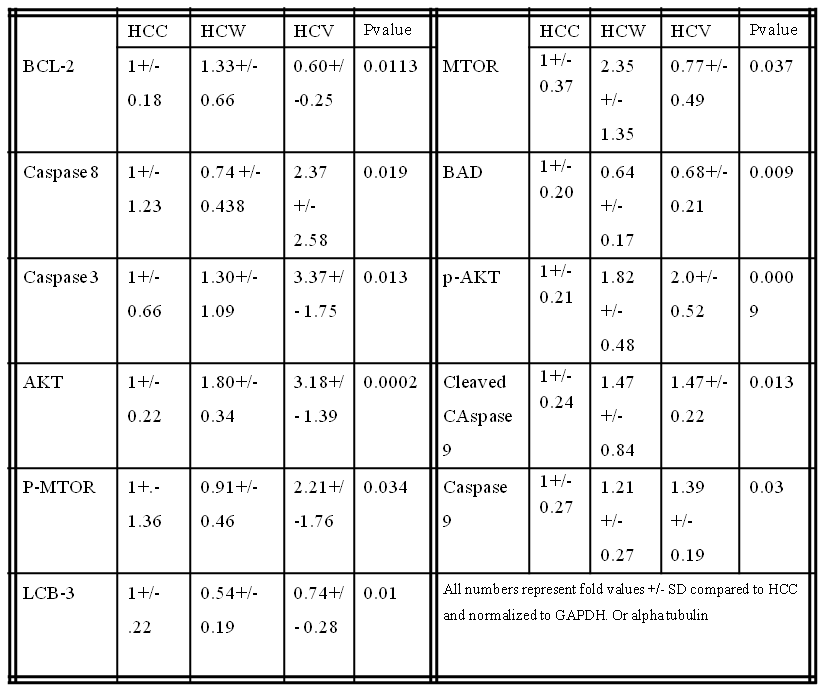
Methods: Liver organoids composed of either hepatocytes alone or hepatocytes co-cultured with stellate cells were generated by 3D culture in rotating wall vessel bioreactors. Primary hepatocytes and stellate cells were isolated from ROSA26 C57BL/6 mice, in which β-galactosidase was expressed under a ubiquitous promoter, so that engrafted cells could be easily identified by X-gal staining when implanted into wild-type mice. Some recipient mice underwent simultaneous two-thirds partial hepatectomy to determine whether hepatocytes within implanted organoids proliferated in response to acute liver insufficiency. As control, freshly isolated primary hepatocytes were transplanted as single-cell suspensions. At various time-points after implantation, engraftment of liver organoids was qualitatively and quantitatively determined.
Results: Confocal microscopy analysis demonstrated that hepatocytes within liver organoids had cortical actin organization and produced extracellular matrix. Organoids maintained their 3D structure up to 7 days after implantation within recipient livers and engraftment efficiency was superior to that of single cells. Generating liver organoids with stellate cell co-culture and performing two-thirds partial hepatectomy on recipient mice did not appear to improve engraftment efficiency.
Conclusion: Implantation of liver organoids generated by 3D tissue culture is promising for development as a novel surgical therapy for ESLD. Further optimization of 3D culture and implantation techniques are required to increase engraftment efficiency.