J. Robinson1,2, A. Valentine2, C. Carney2, D. Fabbri1, G. P. Jackson1,2 1Vanderbilt University Medical Center,Department Of Biomedical Informatics,Nashville, TN, USA 2Vanderbilt University Medical Center,Department Of Pediatric Surgery,Nashville, TN, USA
Introduction: Patient portals are online applications that allow patients and their caregivers to interact with healthcare organizations and view health information. Surgeons conduct growing numbers of online encounters by exchanging messages with patients through such portals. We analyzed a random sample of patient portal communications between patients and surgical providers to determine the types of care provided and complexity of medical decision making associated with patient portal messaging.
Methods: We obtained all message threads (i.e., sets of messages exchanged between patients and providers) initiated by patients and sent to surgical providers through the Vanderbilt University Medical Center patient portal from June 1 to December 31, 2014. Of these, 500 were randomly selected for detailed analysis. Message content was analyzed by two research team members and classified using a validated consumer health taxonomy, including categories for medical, logistical, informational, and social communications. Within each thread, we determined the complexity of medical decision making, one of the three defined elements of outpatient billing, according to the Center for Medicare and Medicaid Services (CMS) Evaluation and Management (E/M) guidelines. Discrepancies in category assignments were discussed to reach consensus.
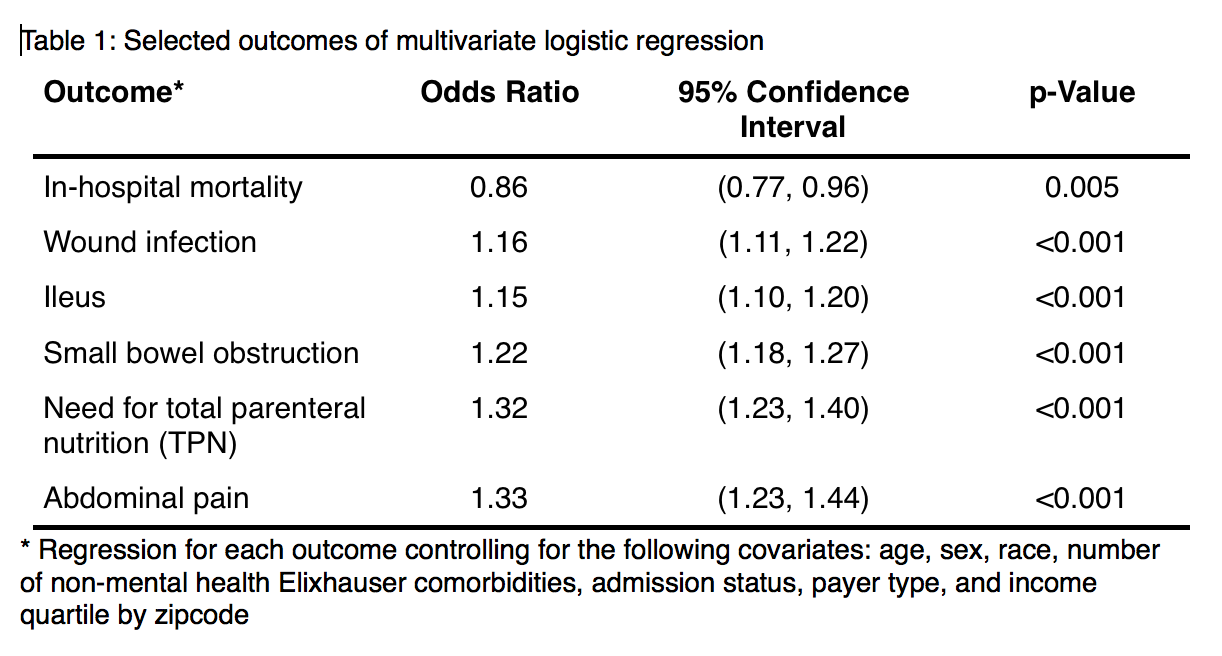
Results: 9,408 message threads were sent to 567 surgical providers during the analyzed period. Of the 500 randomly selected message threads, 1281 distinct issues were communicated, with an average of 2.6 issues per thread. Medical care was delivered in 453 message threads (90.6%) as described in Table 1. Logistical needs, such as contact information or insurance questions, were addressed in 150 threads (30.0 %); health information needs in 77 threads (15.4 %); and social communications (e.g., complaints or emotional needs) in 62 threads (12.4 %). 339 (67.8 %) of message threads contained medical decision making, low risk in 171 (50%) and moderate risk in 132 (39%), with the remaining straightforward or high risk. The overall complexity of medical decision making was straightforward in 62% (210 messages), low in 30% (102 messages), and moderate in 8% (27 messages). No highly complex decisions were made over portal messaging.
Conclusion: Through patient portal messages, surgeons deliver substantial medical care with varied levels of medical complexity. Implementation of patient portals by healthcare systems will continue to increase in response to consumer demand and regulatory pressures such as the Affordable Care Act. Models for compensation of online care must be developed as consumer and surgeon adoption of these technologies increases.