A. D. Kaminski1, G. N. Falls1, P. P. Parikh1 1Wright State University,Department Of Surgery,Dayton, OH, USA
Introduction:
The primary objective of this study was to determine the influence of clerkship experience on specialty choice. Since students only experience six specialty rotations throughout third year, our goal was to determine if the lack of exposure is deterring students from certain specialties. We also identified factors that influence decision of students who choose a specialty that is not a part of third year curriculum.
Methods:
An IRB-approved questions based survey on Qualtrics was prepared and sent to all graduating 4th year medical students at our institution. The survey included questions related to specialty interests before and after clerkships and influence of clerkship experience on specialty choice. Students also provided descriptive response on specific factors influencing their specialty choice and things medical school could do to facilitate their decision. The data were then analyzed descriptively and qualitatively to identify themes.
Results:
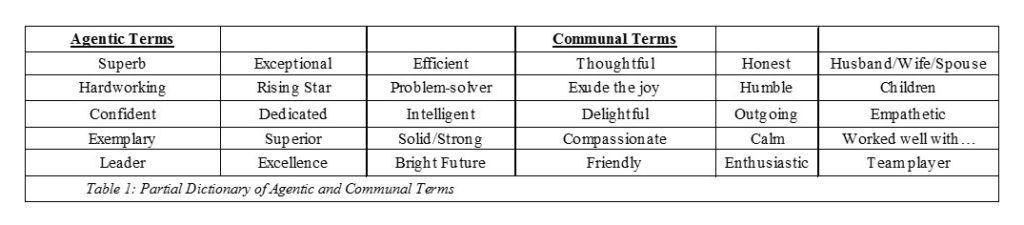
Majority of students (87%) had at least minimal exposure to their chosen specialty prior to the clerkship. This exposure increased significantly following the clerkship (97%). 70% of students reported that the role of clerkship experience in selecting a specialty was either extremely significant or significant. Various aspects of clerkships were influential, as shown in Table 1. Specialty interests before and after clerkships were variable, for example 10 students were interested in surgery prior to clerkships, and 8 decided to pursue surgery as career. The most influential reasons for a student’s specialty choice to change after clerkships, were clerkship experience (56%) and mentors (28%). 34% of students chose a specialty that was not a part of 3rd year clerkships. Of those students, the most significant factors influencing their specialty choice were shadowing experience (65%) and lifestyle (61%). Qualitative analysis of data indicated that students requested earlier and more exposure to various specialties in order to make specialty selection process easier.
Conclusion:
Clerkship experience plays a major role in selecting a specialty. Earlier exposure would help the decision-making process. Students who ultimately choose a non-core specialty would benefit from more shadowing and earlier exposure.