P. J. Lawson1, H. B. Moore2, R. Choudhury2, C. Chang2, A. Kam2, E. Pomfret2, S. Mandell3, J. Pomposelli2, M. Chapman4, T. L. Nydam2 1University Of Colorado Denver,School Of Medicine,Aurora, CO, USA 2University Of Colorado Denver,Surgery-Transplant,Aurora, CO, USA 3University Of Colorado Denver,Anesthesiology,Aurora, CO, USA 4University Of Colorado Denver,Radiology,Aurora, CO, USA
Introduction:
Thrombocytopenia persists following liver transplantation (LT) and platelet recovery after LT remains poorly understood. Therefore, the aim of this study is to characterize the arachidonic acid (AA), thrombin (TRAP), and adenosine diphosphate (ADP) platelet functions during LT, in contrast to clot strength and fibrinogen contributions. We hypothesize that platelets regain functionality following transplantation, but not all agonists at the same time.
Methods:
Whole blood samples were drawn from baseline phase preoperatively through post-operative day 5 (POD5). Eleven liver transplant recipients consented for analysis with both thrombelastograpahy (TEG) and rotational thromboelastometry (ROTEM) platelet aggregometry. Assays included, TEG MA (clot strength), TEG angle (fibrinogen), and platelet counts in addition to platelet aggregometry with added AA, ADP, and TRAP agonists. Platelet function was estimated by the area under the curve (AUC). Measurements were contrasted to five healthy individuals. A paired Wilcoxon test was used to contrast transplant patients over time, and a Mann Whitney test was used to contrast transplant and control samples.
Results:
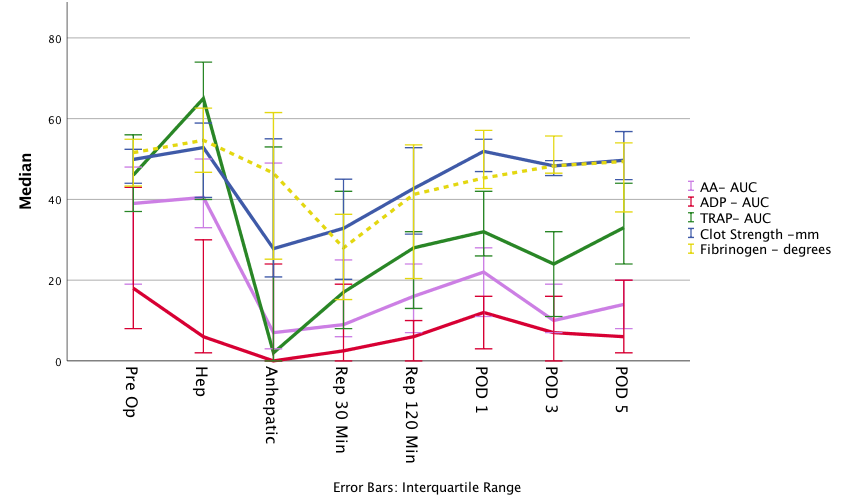
The median MELD score was 18. 64% of patients had baseline platelet counts less than 100,000. Clot strength was lowest during the anhepatic phase (P<0.05), returning to baseline by POD1 through POD5 (figure). Fibrinogen was lowest at 30 minutes after reperfusion (P<0.05), but regained baseline by POD1 (figure). Platelet counts remained low relative to baseline for POD1, 3, and 5 (85,000; 45,000; 51,000; 45,000. P<0.05). Platelet function of all three pathways reached their nadir during the anhepatic phase, and recovery began during reperfusion (figure). Platelet function improved by POD1 in all 3 pathways, but ADP was significantly low for POD3 (p=0.009) and 5 (p=0.036). AA and TRAP functions were depressed from POD1-5 but did not reach significance. Baseline platelet function did not differ from controls, but all three pathways were depressed by POD1 in transplant patients (p<0.05). TRAP regained function comparable to controls by POD5, but AA and ADP remained lower (P<0.001).
Conclusion:
Platelet agonist pathways were not upregulated following surgery in LT recipients. Patients regain baseline clot strength by POD1, despite a lower platelet count and suppressed function. Recovery in clot strength parallels an increase in fibrinogen while platelet function of the ADP and AA pathways remains suppressed through POD5. These measured coagulation derangements during and after LT warrant further investigation as current post-operative anti-thrombotic prophylaxis may be off target.